The 3 Most Common Running Injuries We See in South Delta
There is something special about the running community here in South Delta. Whether you are training for your first 10K on the flat, scenic trails of the Boundary Bay Dyke, tackling the hills near the ferry terminal, or simply enjoying a morning jog around Centennial Beach, running is woven into the fabric of our Tsawwassen lifestyle.
But every runner, from the weekend warrior to the marathon veteran, knows the fear. It starts as a whisper—a slight tightness in the calf or a dull ache in the knee. You ignore it, hoping it will go away. A week later, that whisper becomes a scream, and suddenly, you are sidelined.
At Monument Health Canada, we see this narrative play out constantly. The good news? Most running injuries are not random bad luck. They are predictable, preventable, and highly treatable.
As Tsawwassen’s hub for integrated health, our team of Physiotherapists, Kinesiologists, and Registered Massage Therapists (RMTs) has identified the three most common injuries plaguing local runners. Here is your guide to spotting them early and fixing them for good.
The Golden Rule: "Load vs. Capacity"
Before we dive into the specific injuries, it is crucial to understand why runners get hurt.
In almost every case we treat at our South Delta clinic, the issue boils down to Load vs. Capacity.
Load: The stress you place on your body (distance, speed, hills, footwear).
Capacity: How much stress your tissues can handle (strength, flexibility, recovery).
When Load exceeds Capacity, tissue breaks down, and pain begins. The goal of Physiotherapy isn't just to kill the pain; it is to increase your Capacity so you can handle the Load.
1. Patellofemoral Pain Syndrome (Runner's Knee)
The Feeling: You feel a dull, aching pain around or behind your kneecap (patella). It is often aggravated by running downhill, walking down stairs, or sitting for long periods with your knees bent (the dreaded "movie theater sign").
Why it Happens: Contrary to popular belief, the problem is rarely the knee itself. The knee is a hinge joint—it does what the hip and foot tell it to do. If your glute muscles (hips) are weak or under-active, your femur (thigh bone) rotates internally when you land. This causes the kneecap to track incorrectly in its groove, grinding against the cartilage.
How We Treat It at Monument Health:
Physiotherapy: We assess your hip strength. Often, strengthening the Gluteus Medius helps align the knee instantly. We may also use taping techniques to offload the joint immediately.
Kinesiology: A Kin will analyze your running gait. Are you over-striding? Often, increasing your cadence (steps per minute) reduces the impact force on the knee by up to 20%.
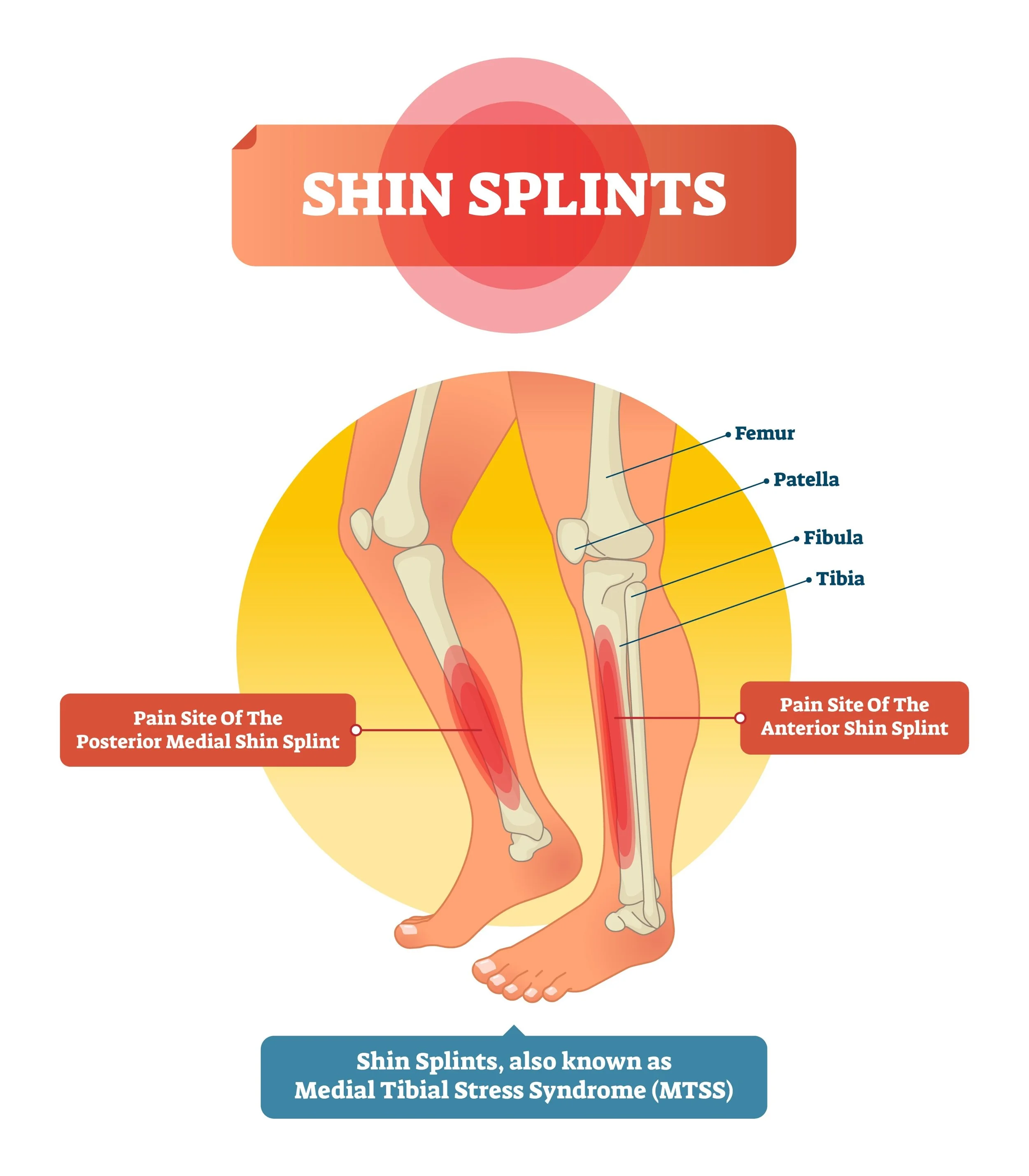
2. Medial Tibial Stress Syndrome (Shin Splints)
The Feeling: A throbbing, tender pain along the inner edge of your shin bone (tibia). It usually hurts at the start of a run, warms up and feels better during the middle, and then throbs uncontrollably once you stop.
Why it Happens: This is the classic "Too Much, Too Soon" injury. We see a spike in Shin Splints in Tsawwassen every January (New Year’s resolutions) and every spring (when the sun comes out). It occurs when the muscles that attach to the shin bone pull too aggressively on the periosteum (the skin of the bone), causing inflammation.
Warning: If ignored, shin splints can turn into a stress fracture. If you have pinpoint pain on the bone that hurts even when walking, book a Physiotherapy assessment immediately.
How We Treat It at Monument Health:
Physiotherapy: We differentiate between muscle inflammation and bone stress. We use modalities to reduce inflammation and manual therapy to loosen the tight calves pulling on the bone.
Massage Therapy (RMT): Tight soleus and gastrocnemius (calf) muscles are the culprits here. Deep tissue release from an RMT can significantly reduce the tension on the shin bone.
3. Plantar Fasciitis
The Feeling: A sharp, stabbing pain in the heel or the arch of the foot. The hallmark sign is that the first few steps in the morning are excruciating, but the pain eases up as you walk around, only to return after sitting for a while.
Why it Happens: The Plantar Fascia is a thick band of tissue connecting your heel to your toes. It acts as a shock absorber. If you have limited ankle mobility (stiff calves) or poor foot mechanics, that band gets overstretched and develops micro-tears. Running on the concrete sidewalks of South Delta or worn-out shoes can exacerbate this rapidly.
How We Treat It at Monument Health:
IMS / Dry Needling: This is often a game-changer for Plantar Fasciitis. By releasing deep trigger points in the calf muscles, we can introduce slack to the system, relieving the tension on the foot.
Kinesiology: We look at your foot mechanics. Do you need to strengthen the intrinsic muscles of your foot? Do you need temporary orthotic support?
Quick Reference Guide: The Runner’s Troubleshooter
Use this table to quickly identify what might be happening.
| Injury | Classic Warning Sign | The Likely Cause | The Monument Health Fix |
|---|---|---|---|
| Runner's Knee (Patellofemoral Pain) |
Pain going down stairs or sitting for long periods. | Weak hips (glutes) causing poor tracking. | Glute strengthening & Gait retraining. |
| Shin Splints (Medial Tibial Stress) |
Inner shin throbs after running, hurts to touch. | "Too much, too soon" & tight calves. | Load management, RMT for calves, & rest. |
| Plantar Fasciitis | Stabbing heel pain with the first steps in the morning. | Stiff ankles & poor arch support. | IMS/Dry Needling & Foot strengthening. |
Prevention: Don’t Wait Until It Breaks
The biggest mistake we see runners in Tsawwassen make is waiting until they cannot walk before they seek help.
Running is a high-impact sport. It requires maintenance. You wouldn't drive your car for 50,000km without an oil change and expect it to run smoothly. Your body is no different.
1. The Pre-Hab Assessment (Physiotherapy)
You don't need to be injured to see a Physiotherapist. A preventative assessment can identify tight hip flexors or weak glutes before they cause Runner's Knee. We can give you a specific "warm-up menu" to keep you safe.
2. Soft Tissue Maintenance (RMT)
Regular visits to a Registered Massage Therapist help keep your tissues pliable. If your calves are supple, they won't pull on your Achilles or your shins. RMT is not a luxury for runners; it is part of the training plan.
3. Form Correction (Kinesiology)
Sometimes, you just need to learn how to run. Our Kinesiologists can take you through a running analysis. Small tweaks—like leaning slightly forward or shortening your stride—can reduce the impact on your joints by massive amounts over the course of a 5km run.
In Conclusion: Keep Running, South Delta!
We live in one of the most beautiful places in British Columbia to be a runner. We want you out there enjoying the fresh air, not sitting at home icing your knee.
If you are feeling that familiar "twinge," or if you are planning to ramp up your mileage for an upcoming race, come see the team at Monument Health. We are passionate about keeping our community moving.
Don't let a simple injury become a chronic problem.
Whether you need a diagnosis from a Physiotherapist, a release from an RMT, or a strengthening plan from a Kinesiologist, we have the tools to keep you on the trails.
Ready to run pain-free?
Disclaimer: This article is for informational purposes only and does not constitute medical advice. If you have severe pain, swelling, or cannot bear weight, please consult a healthcare professional immediately.